
IVF NewsNews: Air Products is the only UK industrial gas supplier to offer liquid nitrogen compliant to the new Medical Device Regulation
Jackie Taylor 24 May 2022

Air Products is the only UK industrial gas supplier to offer liquid nitrogen compliant to the new Medical Device Regulation Air Products is proud to announce that it has been awarded Medical Device Regulation (MDR) EC Mark certificate for Medical Device liquid nitrogen for the UK. Do I need MDR liquid nitrogen? It depends on your application. If it involves the storage of human tissue samples the chances are that you do. This includes any applications that use liquid nitrogen for preserving blood and bone marrow cells, sperm, ova, early embryos, and, in the microbiology laboratory, a variety of microorganisms (bacteria, fungi, etc) Another application that requires MDR liquid nitrogen is cryotherapy, which refers to the focal application of extreme cold for the in-situ destruction of abnormal or diseased tissue. What does MDR Device liquid nitrogen actually mean? Liquid nitrogen that could come into contact with life science samples through cryogenic storage or cryotherapy is classified as a class IIa medical device, compliance with the MDR means that we as the manufacturers need to ensure that:
I have heard of the Medical Device Directive (MDD) but what is the Medical Device Regulation (MDR)? The MDR replaced the MDD in May 2021. The MDR is substantially more comprehensive and detailed compared to the MDD. The MDR document is four times longer than the MDD and puts more emphasis on product safety. Nothing from within the MDD has been removed, rather the MDR has only added new requirements. Air Products have completed months of work to ensure that liquid nitrogen manufactured and supplied within the UK complies with the new more comprehensive Medical Device Regulation. I need MDR liquid nitrogen, how can I get it? Air Products is currently the only industrial gas company manufacturing liquid nitrogen in the UK that complies with the new MDR, contact us today to discuss your requirements. Contact us to discuss your requirements: E: [email protected], T: 0800 164 8512 More information: www.airproducts.expert/uk/biomedical/medical-device-regulation
[ Full Article ] Conference: Embryo-Tech 2.0 Conference (22 & 23 July 2023)
Dr. Keshav Malhotra 24 May 2022

Conference Name: Embryo-Tech 2.0 Conference Date: 22 & 23 July 2023 Venue: The Leela Ambience Hotels & Residences, Gurugram, Delhi NCR About Conference: Increased demand for in vitro fertilization (IVF) due to socio-demographic trends, and supply facilitated by new technologies, converged to transform the way a substantial proportion of humans reproduce. Since its clinical introduction in 1978, in vitro fertilization (IVF) has redefined the ability of the human species to procreate. One of the biggest challenges of this space is to increase pregnancy rates. A lot of technological lab advances have been made in order to achieve the same. Through this conference we will highlight some of the important laboratory advances which help in standardising practices and also smoothens the functioning of the laboratory. Topics like advances in workstations, sperm selection, artificial intelligence, lab management, alarm systems etc would be covered with key faculties at this event. For Registration and Accommodation Query, please contact Mr. Vikas Sharma (+91-9999216837) Email: [email protected] [ Full Article ] Article: Are emerging environmental contaminants a threat to male fertility?
Microptic 23 May 2022
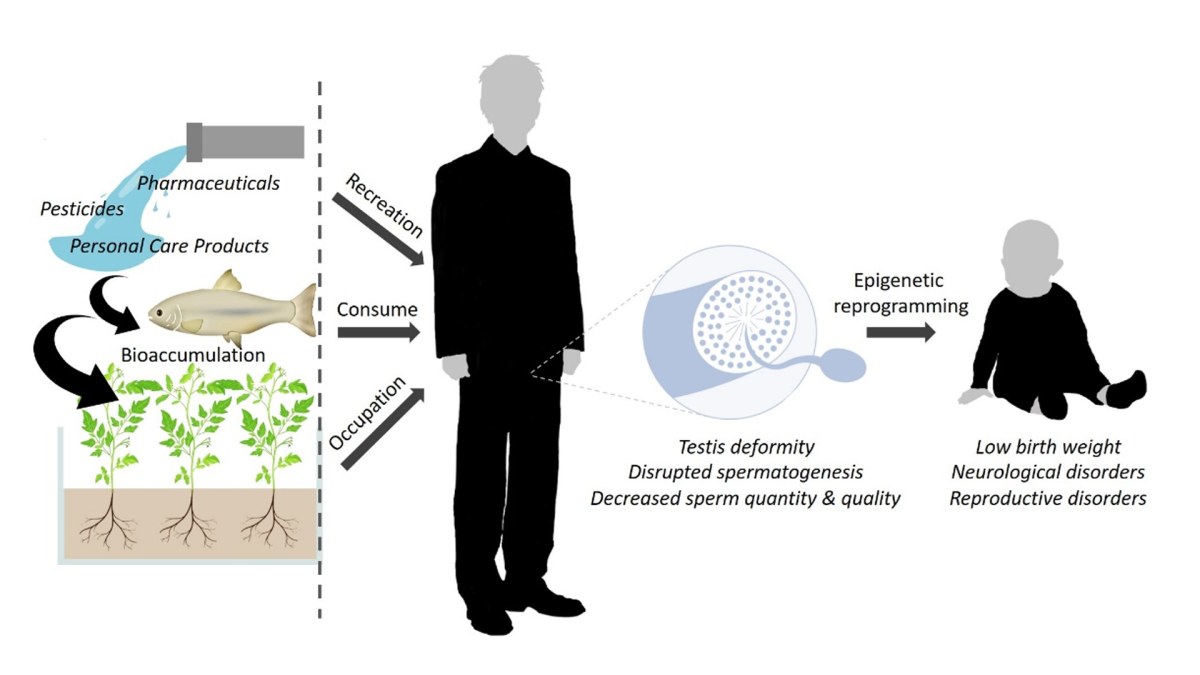
Unexplained male infertility is evident in up to 25% of male factor infertility cases and exposure to environmental contaminants could be one of many culprits in the global decline in male fertility. Since many of these compounds end up in water bodies, it is referred to as Contaminants of Emerging Concern (CECs) and are typically not regulated under current environmental laws. Origin and health impact of CECs One of the main consequences of industrialization is the production, use and discharge of several CECs, including pharmaceuticals, personal care products and pesticides. The presence of CECs is well-documented in a wide range of environmental and food matrices, such as surface water, wastewater, soil, livestock manure, human waste, plants and seafood (Figure 1).
Figure 1: Major sources of emerging contaminants and its distribution to water bodies (adapted from Rasheed et al. 2019). The large-scale use of CECs has resulted in their ubiquitous occurrence in surface and ground water sources and has caused great concern among the scientific community and regulatory authorities in recent years. In addition, current water treatment techniques (e.g. biodegradation, flocculation, ozonation, electrodialysis, reverse osmosis and sedimentation) are not sufficient enough or unable to completely degrade many CECs. As a result, human populations can be exposed to CECs by drinking contaminated water, consuming aquatic species affected by CECs or even recreational activities in affected water bodies. CECs generally refer to compounds that have not previously been detected or only detected in small quantities through water quality analysis and thus the risk they pose to human or environmental health is not yet fully understood. While researchers have started to examine the adverse effects of CEC exposures on human health, including fertility, it has provided varied findings. Many CECs mimic the action of hormones in the body and can disrupt the endocrine system and subsequent basic physiological functions, while others are classified as carcinogens. The prevalent male reproductive side effects of exposure to CECs include gonadal malformations, interference with spermatogenesis, hormone imbalances, and demasculinisation, as was shown for a variety of vertebrates including fish, turtles, birds and mice. In addition, it is suggested that CECs may have a harmful effect on the offspring of affected parents via the inheritance of epigenetic markers. Therefore, parental exposure to the CECs will not only affect the parents themselves but also leave profound signatures in the germline, compromising the health of the next generations (Figure 2).
Figure 2: Effects of contaminants of emerging concern from the source to the offspring of exposed individuals. Recent reports on CECs in the marine environment The Environmental and Nano Science Research Group (Department of Chemistry, University of the Western Cape, South Africa) under the leadership of Prof Leslie Petrik has investigated the occurrence and accumulation of various CECs (including herbicides, pharmaceutical and personal care products) in the marine environment around Cape Town. Many of the CECs detected are most likely due to several wastewater-treatment plants discharging improperly treated effluents into the ocean. Prof Petrik and co-workers reported that the levels of CECs in the seawater, sediment and several marine organisms (seaweed, invertebrates and fish) pose a low acute and chronic risk to various tropic levels due to its bioaccumulation factor and calculated risk quotients. Current investigation on the effect of CECs on sperm function
Figure 3: CEC team in the Comparative Spermatology Group: Daniel Marcu, Shannen Keyser, Liana Maree and Monique Bennett. The Comparative Spermatology Group (Department of Medical Bioscience, University of the Western Cape, South Africa) has joined forces with the Environmental and Nano Science Research Group in deciphering the potential consequence or mechanisms of action of CEC exposure on sperm function in vitro. Two PhD students, Daniel Marcu (School of Biological Science, University of East Anglia, United Kingdom) and Shannen Keyser (Comparative Spermatology Laboratory) (Figure 3), have studied the effects of the most prevalent CECs found in our marine sources on human sperm function, including anti-inflammatory and antibiotic drugs, as well as some herbicides, using computer-assisted sperm analysis (CASA). One of the advantages of CASA is that it allows the researcher to visualize, evaluate and obtain precise information on the swimming characteristics of individual sperm. CASA applications are limitless, and they provide instrumental insights in reproductive toxicology and human fertility. Understanding the specific kinematics and the molecular events underpinning them is of great importance for establishing toxicology level cut-offs for sperm function. Our preliminary results after sperm from donor samples were chronically exposed to several contaminants indicate that the various chemicals disrupt the sperm plasma membrane and metabolic processes. While exposure to the CECs typically decreased the percentage total and progressive motility (Figure 4), more significant adverse effects were found on the kinematic parameters (such as VAP, VSL and BCF), especially in that of the slow and medium progressive speed groups. It was further noted that some of the CECs has varying effects on different motility sperm subpopulations. We are in the process of also assessing its effect of other sperm functional parameters, e.g. vitality, hyperactivation and acrosome reaction.
Figure 4: Motility parameters of a high motile sperm subpopulation of after 30 minutes exposure to various concentrations of the non-steroidal anti-inflammatory Naproxen. Apart from using human sperm to investigate the effect of CECs on sperm function, we also embarked on studying its effect on sperm from broad cast spawners, such as sea urchin and oyster. These species are presumably directly affected by the exposure to contaminants in their marine environment and are known to bioaccumulate CECs. Such testing could in future act as a warning system that identifies the causes of population decline in animal populations, offering potential interventions for conservation of entire ecosystems. Through our investigations, we also hope to increase public awareness about the threat of CEC exposure to the environment and human health. Dr Liana Maree (PhD) Daniel Marcu (PhD Candidate) Shannen Keyser (PhD Candidate) [ Full Article ] Webinar: AI - UNDER THE HOOD
International IVF Initiative 23 May 2022

Tuesday, 24th May at 3pm EST, 8pm UK, 9pm CET [ Full Article ] News: HFEA considers proposing donor anonymity law changes
Hannah Flynn 23 May 2022
The Human Fertilisation and Embryology Authority (HFEA) is considering ways gamete donor anonymity laws could be changed, as the advent of straight-to-consumer genetic testing has 'thrown into question' the assumption of anonymity. Speaking to the Guardian newspaper HFEA chief executive Peter Thompson said that genetic testing from websites such as 23andMe and Ancestry were making it impossible to preserve the anonymity of donors. This meant that the Authority was considering changing the law first introduced in 2005 in the UK, which currently allows donor conceived people to access identifying information about their donor parent at the age of 18, but not before. He told the Guardian: 'Given the trend, I can't see how the existing legal framework is going to cope with the way things are going.' The HFEA is planning to consult on and propose legislative changes by the end of the year, and was considering how to deal with the question of donor anonymity in the face of ubiquitous genetic testing. Thompson told the Guardian one option being considered was 'a presumption of openness almost from the word go'. However, the exact timing of the removal of anonymity was an important point said Progress Educational Trust director Sarah Norcross: 'Any changes to the timing of donor identity release will give rise to a number of complex issues, and will fail to satisfy everyone.' Instead she urged that HFEA take note of the fact that donors, fertility patients and their children are a diverse group of people with different needs, and changes in legislation need to reflect this. Imposing a single model should be avoided, she said: 'Just because early identification of donors has become more likely, does not mean that this should become a legal requirement. Making donors mandatorily identifiable earlier in the process may cause more problems than the HFEA hopes to solve. Will the donor be identifiable to the intended parent(s)? If so, at what point in the treatment pathway? For example, will this become part of the process of choosing a donor? Or will the donor's identity only be released once a child is born?' 'Who will be responsible for the release of this information, and for associated support services? Who will pay for these services? What will be the impact on people's willingness to donate? Will fertility patients become more likely to seek treatment overseas, where such rules do not apply?' Thompson argued changing the law to remove anonymity was unlikely to affect people's willingness to donate gametes, and pointed out that similar concerns had been voiced when the law was first changed to remove anonymity in 2005. An initial dip in donations occurred, and then recovered. 'There's no hard evidence that you would lose donors.' he told the Guardian. SOURCES & REFERENCES [ Full Article ] News: HFEA reports on IVF access during the COVID-19 pandemic
Cliona Farrell 23 May 2022
NHS-funded IVF cycles were slower to resume on average than privately-funded treatments after the mandatory closure of all UK clinics due to the COVID-19 pandemic. Fertility treatments were suspended by the government three weeks into the first national lockdown due to the impact that COVID-19 was having on the NHS, and the then-unknown risks of the virus to pregnant women. A new report from the Human Fertilisation and Embryology Authority (HFEA) shows that NHS clinics were slower to resume, with only 34 percent reopening on the first permitted day, compared to 83 percent of private clinics. 'Many patients wanted to begin or continue fertility treatment during the pandemic and clinic staff went above and beyond to offer safe care,' said HFEA chair Julia Chain. 'However, COVID-19 related measures did impact some patients, as many appointments had to be provided remotely and those that were in person, were restricted in attendance to just the patient.' Fertility clinics were told to close in April 2020 and could apply to reopen from 11 May if a safe environment could be created for patients and staff. Total NHS-funded IVF treatments fell by seven percent in 2020, compared to 2019. Reasons that NHS treatment was more seriously impacted may include staff redeployment to other areas of the NHS, and that many NHS fertility clinics are located within hospitals treating COVID patients and may have had to take extra precautions around social distancing. The new report shows that IVF cycles in patients between 18-34 years decreased more than that of patients aged 40-50, likely due to clinics prioritising older patients as the probability of successful treatment decreases with age. Those in heterosexual relationships experienced a greater decrease in IVF cycles in 2020 compared to those in same-sex relationships. This may be because of the larger proportion of NHS-funded fertility treatment for heterosexual couples. Embryo storage was the only area in which an increase over 2019 was observed. The report echoes findings of the HFEA patient survey published by the HFEA last month which found that NHS-funded patients were twice as likely to report experiencing delays in starting IVF treatment than privately funded patients. 'These figures confirm our fears that the double whammy of poor NHS funding and the COVID pandemic had a devastating impact on UK fertility patients,' said Sarah Norcross, director of the Progress Educational Trust. 'Privately funded IVF cycles not only matched but exceeded 2019 levels by mid-2020, whereas NHS-funded cycles had yet to return to 2019 levels by mid-2021. It is yet unclear whether the situation has improved since then.'
SOURCES & REFERENCES
[ Full Article ] News: Sperm epigenetics linked to likelihood of pregnancy
Daniel Jacobson 23 May 2022
A new method for determining the 'biological age' of sperm may be a useful predictor of pregnancy success. A study conducted at Wayne State University School of Medicine, Detroit, Michigan, and published in the journal Human Reproduction, found a 17 percent decrease in reproductive success after twelve months of trying to conceive for couples with a male partner with biologically 'older' sperm. This method was based on levels of methylation in sperm which are known to accumulate with age, known as an 'epigenetic clock'. 'Chronological age is a significant determinant of reproductive capacity and success among couples attempting pregnancy, but chronological age does not encapsulate the cumulative genetic and [environmental …] factors' said Dr Richard Pilsner, the lead author of the study. '[An epigenetic clock] serves as a proxy measure of the "true" biological age of cells.' The study included 379 US couples from the Longitudinal Investigation of Fertility and Environment Study, where DNA methylation analysis was conducted on the sperm of the male partner. Partners had not undergone fertility treatment previously but had been off contraception with the intention of becoming pregnant. The study findings were also validated in an independent IVF cohort. While the chronological and epigenetic ages were strongly correlated, the study reiterated that the latter would capture various features which drive methylation and may enhance pregnancy success prediction. For example, smokers, on average, showed higher sperm epigenetic ages, demonstrating the additional information provided by this measure. The authors argue that a sperm epigenetic clock may be useful as a future biomarker of reproductive success, and that the study specifically highlights the importance of the male partner in determining this. Additionally, it is hoped that this tool might inform decisions surrounding potential infertility treatment at early stages. 'Semen quality outcomes utilising World Health Organisation guidelines have been used to assess male infertility for decades, but they remain poor predictors of reproductive outcomes', said Dr Pilsner. 'The ability to capture the biological age of sperm may provide a novel platform to better assess the male contribution to reproductive success, especially among infertile couples.' SOURCES & REFERENCES
[ Full Article ] News: Colorado bans anonymous sperm and egg donation from 2025
Jen Willows 23 May 2022
Colorado has passed a bill that will give donor-conceived people the right to access information about their donors. If Governor Jared Polis signs the bill into law, the 'Donor-conceived Persons and Families of Donor-conceived Persons Protection Act' will allow all children conceived with donor gametes from 2025 onwards to access medical history and identifying information about their donor when they turn 18. 'We want to make clear that someone whose donating sperm or egg will no longer be anonymous,' said Representative Matt Soper, who sponsored the bill. 'Through technologies that are out there, they need to understand what the ramifications are of making the decision to be a donor'. The bill also brings in regulations requiring sperm banks and fertility clinics to be licensed and to maintain records of donors' medical records and contact details as well as children born from each donor. The number of families that can be created from a single gamete donor will be limited to 25, and egg donors will be limited to a maximum of six egg retrieval cycles. Part of the rationale for this bill is the availability of commercial DNA testing companies that allow donor-conceived people to find out they are genetically linked to people they may not have expected, as well as connect to genetic half-siblings who share the same donor. 'As the technology makes it easier for people to find out that their legal parents are not their genetic parents, there is increasing interest among donor-conceived people to have access to this information,' said Professor Naomi Cahn who specialises in family law at the University of Virginia. Some people have discovered larger numbers of half-siblings, which is why the bill seeks to limit the number of families each donor can help. In 2011 Washington became the first state to allow donor-conceived people access to their donor's identity and medical history from age 18, and others have followed, but all permit donors to opt out of having their details shared. If the bill is signed, Colorado would be the first to remove that option. The act will not be retroactive, however, so donors of children already born, or who will be conceived before 2025 will be able to remain anonymous. One concern that was voiced in opposition to the bill is that the removal of anonymity could mean that fewer people are willing to donate in future. However, through direct-to-consumer genetic testing many people are able to identify their donor anyway: 'The promise of anonymity is elusive,' said Professor Cahn. 'Yes, a clinic can promise not to reveal that information, but that then doesn't mean that someone who engages in this genetic testing won't then find the donor and perhaps reach out.' SOURCES & REFERENCES
[ Full Article ] News: Rat testicle cells frozen for 23 years make sperm
David Cansfield 23 May 2022
Rat testicle stem cells that were frozen for 23 years and then grafted onto infertile mice, have been shown to produce viable sperm. The possibility that pre-pubertal boys could freeze testicular tissue before cancer treatment that might affect their fertility so that it could be grafted on later and allow them to have children is being explored by scientists. This is similar to the ovarian tissue grafts that are offered to pre-pubertal girls who are not able to undergo egg collection before treatment. 'The findings are critical in considering transplantation of stem cells from testis biopsies obtained from prepubertal boys undergoing cancer treatment for later use in re-establishing spermatogenesis following recovery,' said Professor Ralph Brinster, study lead and professor of reproductive physiology from Pennsylvania University Veterinary Medicine department. While sperm can be collected and frozen prior to cancer treatment in adult males, this is not an option for pre-pubescent boys, who cannot yet produce sperm. In this study, published in PLOS Biology, testicular stem cells taken from adult rats and frozen 23 years ago were reintroduced into infertile mice that had been treated with a drug that killed their sperm-making cells. Researchers also carried out the experiment with testicular cells frozen between one to four months ago and with fresh testicular cells. They found that just five to ten percent of these long-term frozen cells were viable, but that after being implanted into mice did differentiate into viable sperm, albeit at a lower rate than fresh or briefly frozen cells. However, even the low sperm count is found to be encouraging if it works in humans who could undergo IVF. 'You really only need one viable sperm to succeed,' Dr Eoin Whelan, one of the authors of the study, explained. Although the rat has long been an important animal model to compare to human physiology, and the process of rat male germ cells differentiation is well understood, it is unclear yet if the results will translate to humans. In addition, the study investigated isolated cells taken from adult rats, while fertility clinics take whole tissue samples from children who have not yet gone through puberty. Those children do not yet know the chance of success of testicular rejuvenation when they consent to undergoing procedures to take a tissue sample before cancer treatment. This is as they may not undergo reimplantation of the tissues for decades and it is not known how well it will survive or be able to differentiate and produce mature sperm. 'I think the research has broad relevance to freezing of all types of stem cells, which could undergo similar changes in gene regulation,' said Professor Brinster. SOURCES & REFERENCES
[ Full Article ] News: Man seeks High Court ruling to use frozen embryos after wife's death
Cliona Farrell 23 May 2022
A widower is seeking High Court approval to use a single remaining embryo he created with his deceased wife, for which he has no written consent. Ted Jennings and his wife, Fern-Marie Choya, underwent multiple rounds of IVF before her death in 2019. Choya conceived twins by IVF but died from a uterine rupture 18-weeks into the pregnancy. The couple had one remaining frozen embryo and Jennings wants to use this in treatment with a surrogate. Representing Jennings, Jenni Richards QC told the judge 'The evidence is that Ms Choya would have wanted Mr Jennings to be able to use their partner-created embryo in treatment with a surrogate in the event of her death.' She argued, however, that Choya 'had no opportunity, through no fault of her own, to provide that consent in writing'. The Human Fertilisation and Embryology Authority (HFEA), which regulates IVF treatment, states that without written consent it is not lawful that an embryo be used posthumously. Prior to their IVF treatment, Jennings gave written consent for the use of the embryos in the event of his death. His wife was not provided with the equivalent question on her consent form, and thus, did not give her consent for this. Instead, her consent form indicated she should speak to the clinic about this option. Jennings and Choya undertook three cycles of IVF treatment in 2013 and 2014 but did not become pregnant. Choya conceived naturally in 2015 and 2016, but both pregnancies ended in miscarriage. The couple underwent further IVF cycles in 2017 and 2018, the latter of which resulted in her pregnancy with twins. Representing the HFEA, Kate Gallafent QC acknowledged that they were sympathetic to Jennings' application but believed the case should be dismissed. 'It is common ground between parties that Ms Choya did not provide written consent to the embryo being used by Mr Jennings in treatment with a surrogate in the event of her death'. She said that the HFEAs 'sole interest' was to 'promote compliance' with a 'statutory scheme'. The judge will provide a written ruling on this case soon. SOURCES & REFERENCES
[ Full Article ] |